What is MRD?
What is MRD?
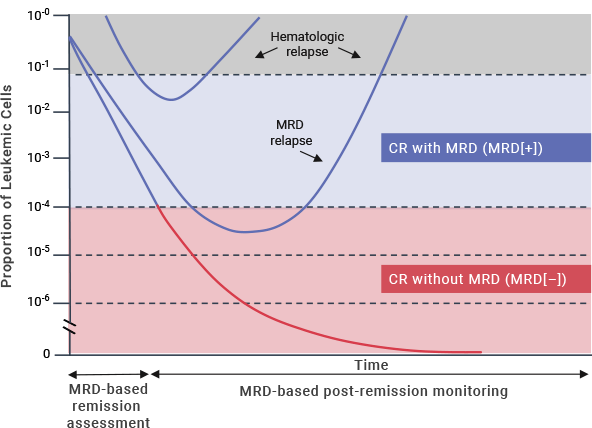
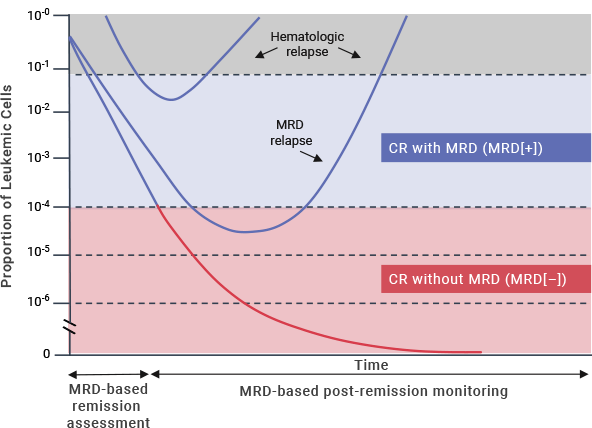
Measurable residual disease (MRD) refers to the presence of leukemic cells below the threshold of
detection when using conventional morphologic methods.1,2 While there is no consensus on a
precise definition of MRD positivity, a sensitivity threshold of 10–4 has been used to
predict patient outcomes.3
Complete remission (CR) is typically defined as < 5% bone marrow blasts.3 A substantial
proportion of adult patients with ALL relapse despite achieving CR, with a reported relapse rate of
40%–50%.4 Furthermore, patients who achieve CR according to morphologic assessment alone may
harbor some residual cancer cells in the bone marrow, with 30%–40% testing positive for
MRD.5,6,*
MRD
and risk of relapse7
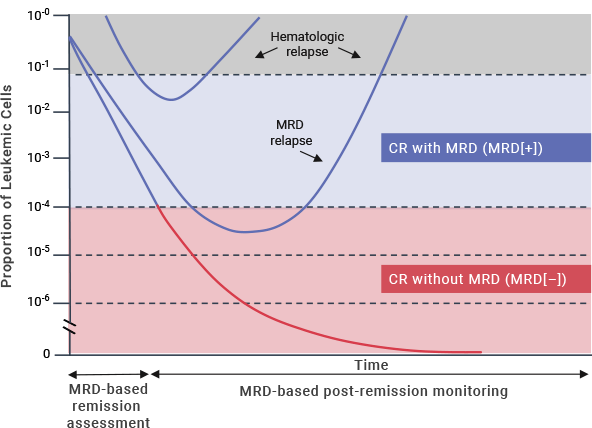
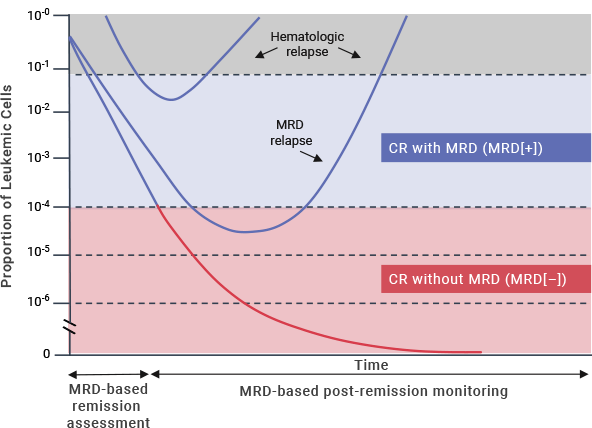
Research continues to lead to an improved
understanding of the impact of MRD on patient prognosis and outcomes.8
 Why is MRD
Why is MRD
important?
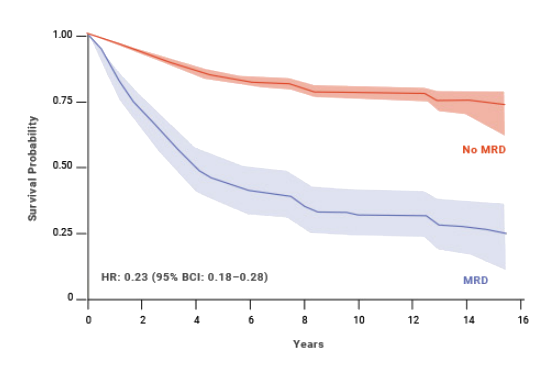
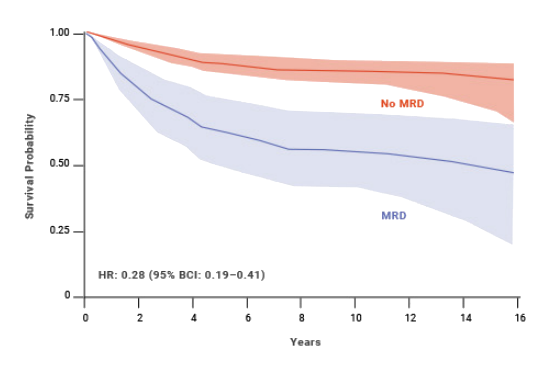
A meta-analysis (Berry et al, 2017) assessed the presence of MRD after induction and consolidation
therapy and concluded that MRD positivity was associated with negative outcomes regardless of
treatment.8
According to the Berry meta-analysis, the presence of MRD is a strong predictor of relapse, which leads
to limited treatment options and poor patient outcomes.8 Achieving MRD(–) status early in the
course of treatment has been shown to give patients a reduced risk of relapse and a stronger chance for
longer overall survival.8
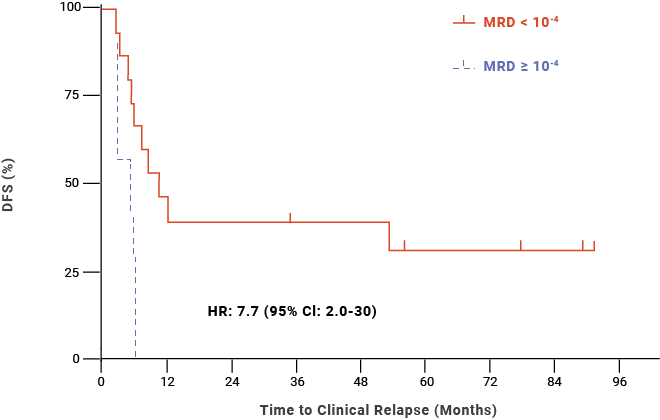
MRD status may be a prognostic factor for post-HSCT outcomes
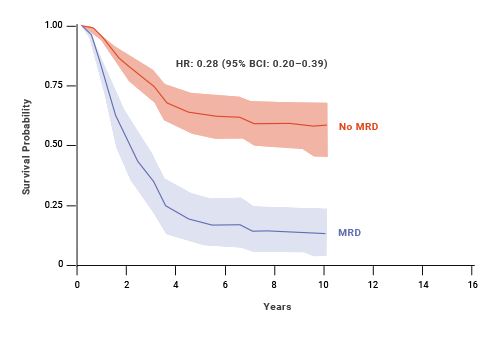
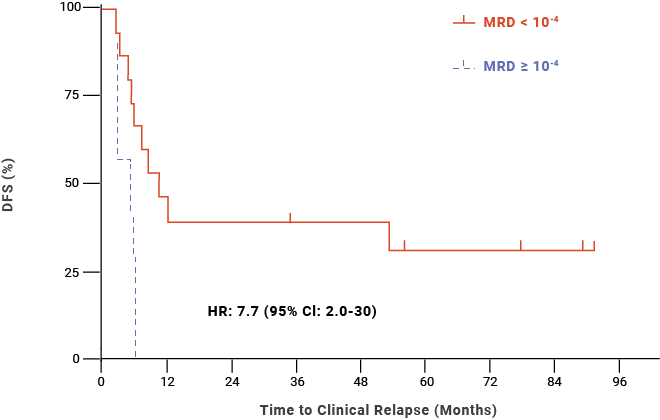
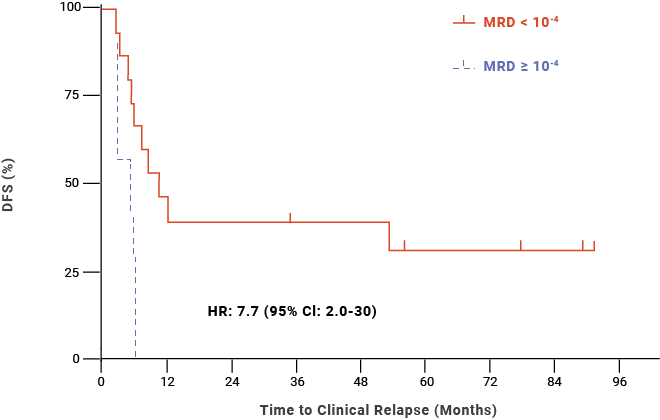
A retrospective study (Logan et al, 2014) analyzed the contribution of MRD in the survival of 29 patients ages 16 to 67 years with B-cell ALL who proceeded to HSCT between 2004 and 2010.9
- In 22 patients with evaluable blood samples, this study found that MRD ≥ 10-4 within 30 days prior to HSCT was associated with relapse post-HSCT in adult/AYA patients with B-cell ALL9,††
Post-HSCT DFS probability for adult/AYA patients with B-cell
ALL9,††
Watch Jae Park discuss the
prognostic value of MRD
Jae Park, MD
Associate Attending Physician
Memorial Sloan Kettering Cancer Center
There remains ongoing research on emerging concepts of measurable residual disease (MRD) in acute
lymphoblastic leukemia (ALL), including MRD cutoff levels appropriate for prognosis and treatment decisions,
standardization of MRD testing methodologies, the use of peripheral blood versus bone marrow to quantify
MRD, and identification of optimal time points for MRD testing. Additionally, the prognostic implications of
MRD status may vary during a patient’s treatment journey (eg, in early assessment versus post-remission
monitoring).10
Your patients may want to learn more about measurable residual disease (MRD). When treating patients who have
achieved remission, it can be helpful to explain that a relatively small number of cancer cells remain in
their body. This is called measurable residual disease, or MRD.11
As a clinician, you have most likely had the challenge of communicating the complexity of disease, potential
relapse, and the rationale for your next steps in treatment in a way that puts patients at ease. In the case
of MRD, you may already have an explanation established that resonates well, or you can consider explaining
that MRD means that, even though they may not have signs or symptoms of cancer, there is a chance the cancer
can return, which is called a relapse.11,12 If your patients test positive for MRD, it may be
encouraging to tell them that there are treatment options that can help them eliminate these small traces of
cancer.3 MRD positivity during treatment may also help inform important decisions, such as the
role of bone marrow transplantation.11
References: 1. Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Acute Lymphoblastic Leukemia V.1.2022. © National Comprehensive Cancer Network, Inc. 2022. All rights reserved. Accessed April 26, 2022. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way. 2. Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Pediatric Acute Lymphoblastic Leukemia V.1.2022. © National Comprehensive Cancer Network, Inc. 2021. All rights reserved. Accessed April 26, 2022. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way. 3. Akabane H, Aaron AC. Clinical
significance and management of MRD in adults with acute lymphoblastic leukemia. Clin Adv Hematol
Oncol. 2020;18:413-422. 4. Hoelzer D. Monitoring and managing minimal residual
disease in acute lymphoblastic leukemia. Am Soc Clin Oncol Educ Book. 2013;33:290-293. 5. Gökbuget N, Kneba M, Raff T, et al. Adult patients with acute lymphoblastic leukemia
and molecular failure display a poor prognosis and are candidates for stem cell transplantation and targeted
therapies. Blood. 2012;120:1868-1876. 6. Brüggemann M, Raff T, Flohr T, et al.
Clinical significance of minimal residual disease quantification in adult patients with standard-risk acute
lymphoblastic leukemia. Blood. 2006;107:1116-1123. 7. Short NJ, Jabbour E,
Albitar M, et al. Recommendations for the assessment and management of measurable residual disease in adults
with acute lymphoblastic leukemia: A consensus of North American experts. Am J Hematol.
2019;94:257-265. 8. Berry DA, Zhou S, Higley H, et al. Association of minimal residual
disease with clinical outcome in pediatric and adult acute lymphoblastic leukemia: a meta-analysis. JAMA
Oncol. 2017;3:e170580. 9. Logan AC, Vashi N, Faham M, et al. Immunoglobulin
and T cell receptor gene high-throughput sequencing quantifies minimal residual disease in acute
lymphoblastic leukemia and predicts post-transplantation relapse and survival. Biol Blood Marrow
Transplant. 2014;20:1307-1313. 10. Brüggemann M, Kotrova M. Minimal residual
disease in adult ALL: technical aspects and implications for correct clinical interpretation. Blood
Adv. 2017;1:2456-2466. 11. Brüggemann M, Gökbuget N, Kneba M. Acute
lymphoblastic leukemia: monitoring minimal residual disease as a therapeutic principle. Semin Oncol.
2012;39:47-57. 12. National Cancer Institute. NCI Dictionary of Cancer Terms.
https://www.cancer.gov/publications/dictionaries/cancer-terms/def/relapse. Accessed November 30, 2021.
 What is MRD?
What is MRD?
 Why is MRD
Why is MRD